I recently visited the dentist for my regular six-month cleaning and checkup.
One mysterious practice you might recall from your own checkup is your hygenist probing around your gums with a pick, while calling out a bunch of numbers that someone else dutifully records in a computer.
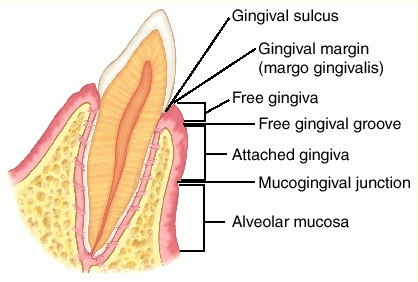 This isn’t some mysterious rite of Dental Magick: they’re measuring the depth of each gingival sulcus—the space between your tooth and your gums. Ideally, in a healthy mouth with healthy gums, this space is approximately 2mm deep, a depth easily reachable and cleanable by regular brushing.
This isn’t some mysterious rite of Dental Magick: they’re measuring the depth of each gingival sulcus—the space between your tooth and your gums. Ideally, in a healthy mouth with healthy gums, this space is approximately 2mm deep, a depth easily reachable and cleanable by regular brushing.
However, most people do not have a healthy mouth with healthy gums. Somewhere between 30 and 50% of the US population has mild periodontitis (inflammation of the gums), with approximately 10% having severe periodontitis.
Plaque and Periodontitis: A Vicious Cycle
The usual cause of periodontitis is dental plaque (a bacterial biofilm), which accumulates in the gingival sulcus. The resulting inflammation causes the sulcus to deepen, beginning a vicious cycle: more plaque = more inflammation = deeper gingival sulcus = more plaque.
A depth of 4mm or more almost always indicates a degree of permanent damage and chronic infection, and is termed a periodontal pocket. Since pockets deeper than 3mm are generally too deep to clean by brushing one’s teeth at home, they tend to become deeper and worse over time, leading to chronic periodontitis—and a depth of 7mm creates a strong risk of tooth loss.
Periodontitis Causes Constant, Low-Grade Inflammation
Even if the pockets never reach this depth, the continual low-grade oral infection of periodontitis (known colloquially as “gum disease”) causes systemic inflammation. We know this is a causal relationship, not just a correlation, because successful treatment of patients with severe periodontitis results in lower CRP and IL-6 levels:
J Clin Periodontol. 2004 May;31(5):402-11.
Periodontitis and atherogenesis: causal association or simple coincidence?
D’Aiuto F, Parkar M, Andreou G, Brett PM, Ready D, Tonetti MS.“A median decrease in serum CRP of 0.5 mg/l (95% CI 0.4-0.7 mg/l) was observed 6 months after completion of periodontal therapy in this population.”
Also see:
J Periodontal Res. 2004 Aug;39(4):236-41.
Periodontal disease and C-reactive protein-associated cardiovascular risk.
D’Aiuto F, Ready D, Tonetti MS.
Given this, the strong association of periodontitis (“gum disease”) with deaths from coronary heart disease (= CHD, = “atherosclerosis”, = the blockage of the coronary arteries due to arterial plaque) should not be surprising.
J Periodontol. 2007 Dec;78(12):2289-302.
Markers of systemic bacterial exposure in periodontal disease and cardiovascular disease risk: a systematic review and meta-analysis.
Mustapha IZ, Debrey S, Oladubu M, Ugarte R.RESULTS: Periodontal disease with elevated markers of systemic bacterial exposure was associated strongly with CHD compared to subjects without PD, with a summary odds ratio of 1.75 (95% confidence interval (CI): 1.32 to 2.34; P <0.001). This group was not associated with CVD events or with stroke but was associated with a significant increase in mean CIMT (0.03 mm; 95% CI: 0.02 to 0.04).
In further support, periodontitis is associated with lower HDL, higher LDL, and increased non-fasting blood glucose:
J Clin Periodontol. 2007 Nov;34(11):931-7. Epub 2007 Sep 17.
Severe periodontitis is associated with systemic inflammation and a dysmetabolic status: a case-control study.
Nibali L, D’Aiuto F, Griffiths G, Patel K, Suvan J, Tonetti MS.
Summary: Our Story So Far
- Dental plaque is a bacterial biofilm that accumulates on our teeth.
- Plaque causes tooth decay—because of the acids the plaque bacteria produce when they ferment sugars in our mouth.
- A gingival sulcus (the space between tooth and gum) deeper than 3mm allows plaque to accumulate unmolested by regular brushing. Its ideal depth is 2mm.
- Plaque accumulation is usually a vicious cycle: more plaque = more inflammation = deeper gingival sulcus = more plaque.
- A sufficiently deep sulcus is known as a periodontal pocket, which usually leads to periodontitis (“gum disease”), and sometimes tooth loss.
- Periodontitis causes systemic inflammation. It is associated with increased risk of heart disease, and with several bad metabolic markers.
Result: we would like all the measurements our dental hygenist calls out to be 2s (signifying a depth of 2mm), with perhaps a few 3s.
A Paleo Diet And My Own Gum Health: Some N=1 Data
I’ve cautioned about extrapolating based on personal experience (“N=1”) before, so I’ll preface this with “correlation is not causation, etc.” However, my warning applies primarily to proving the negative: just because something doesn’t make us feel bad or kill us within a few months doesn’t mean it’s either harmless or good for us!
If we take objective measurements and/or a consistent record of our observations, though, and are careful to evaluate possible confounders (was it that I started eating liver and pastured eggs, or that I got a new job and am sleeping better now that I don’t have to worry about making rent?), it’s often reasonable to correlate improvements with changes we’ve made.
To that end, here is some fascinating data I was able to obtain from my dentist’s office. I think the data is reasonably solid: my measurements were all taken by the same hygienist in the same office, I’ve used the same Sonicare toothbrush and kept the same program of indifferent dental hygiene, and my diet hasn’t changed radically.
Links updated 10/13!
Note that there are several different types of Sonicare toothbrushes: the type I linked above works best, is easiest to clean, and its battery lasts the longest. And if you need two, here’s a two-pack at a discount.
Also note that I was already eating a strongly anti-inflammatory diet previous to “going Paleo”: I had independently found the original research on n-3/n-6 ratio, and had long since removed all seed oils from my diet (I was rendering my own beef tallow back in 2007!) The major dietary changes were going gluten-free, grain-free, and legume-free (except for occasional white rice), and dramatically decreasing my carbohydrate intake—mostly as a consequence of no longer eating bread or pasta.

I went Paleo between the first and second measurements. Therefore, the first set of measurements (#1 on the far left) is my pre-Paleo baseline.
Each tooth is measured six times: at the center and each edge, both front and back. Thus, there are 28x2x3 = 168 such measurements if your wisdom teeth have been removed, 192 if you still have them. For those interested in the raw data, here’s a scan:
Result: starting from a reasonably healthy mouth and an already strongly anti-inflammatory baseline diet, my oral health has improved dramatically—to the point that my dentist told me “Your teeth are great! Whatever you’re doing, keep doing it.”
I have also experienced subjective improvements. My teeth are much less sensitive than before: I used to dread the approach of the electric tooth scaler at each cleaning (it was painful to the point that I would white-knuckle the armrests) but now it doesn’t bother me at all. They’re far less sensitive to cold as well, and less prone to bleeding when I neglect to floss for days or weeks.
In short, while I can’t rule out coincidence, it certainly appears that my excellent dental health is strongly correlated with eating like a predator.
Live in freedom, live in beauty.
JS


